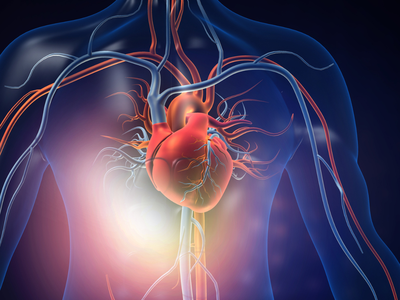
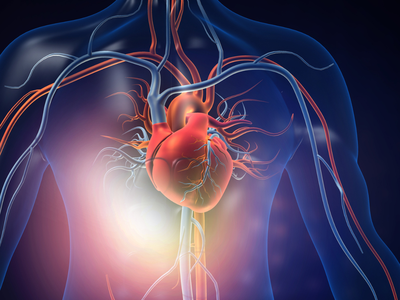
When we think of a heart attack, most of us picture someone clutching their chest in severe pain. But here’s the truth that often gets overlooked: for many women, heart attacks don’t look anything like that. Instead of the classic crushing chest pain, women may feel something as simple as unexplained fatigue, indigestion, breathlessness, or discomfort in the jaw or back. These signs can be so subtle and confusing that they’re easy to brush off as stress, acidity, or just “not sleeping well.”Because women’s symptoms are different and less obvious, heart attacks in women are more likely to go unnoticed or misdiagnosed, sometimes with tragic consequences. And to make things tougher, women often put their own health last while managing work, home, and family, ignoring warning signals until it’s too late.
That’s why it’s crucial for women to understand what silent heart attack symptoms look like and learn to speak up when something feels “off”, says Dr Ravindranath Reddy D R, HOD & Sr Consultant- Interventional Cardiology, Gleneagles BGS Hospital, Kengeri, Bengaluru. Knowing the signs, trusting your instincts, and getting regular preventive screenings can genuinely save lives, he shares in an exclusive interview with TOI.
Why are women more likely to experience silent or less obvious heart attack symptoms than men?
Dr Ravindranath Reddy: In women, heart attacks often present differently than the “classic” chest pain we associate with men. This difference is partly biological and partly due to how women’s heart disease has historically been under-recognized. In women, heart disease often involves the smaller blood vessels rather than the larger arteries, a condition referred to as microvascular disease. Because of this, the symptoms tend to be more subtle and widespread, making them harder to recognize. Hormones also play a role—estrogen offers some protection before menopause, but as its levels drop afterward, a woman’s risk of developing heart disease rises. Additionally, many women juggle multiple roles and tend to attribute symptoms like fatigue, indigestion, or breathlessness to stress or routine exhaustion rather than a possible cardiac issue. Unfortunately, because their symptoms are less dramatic, women are more likely to delay seeking help, which leads to worse outcomes compared to men.
What are the most common “silent” symptoms women should watch for—but often ignore?
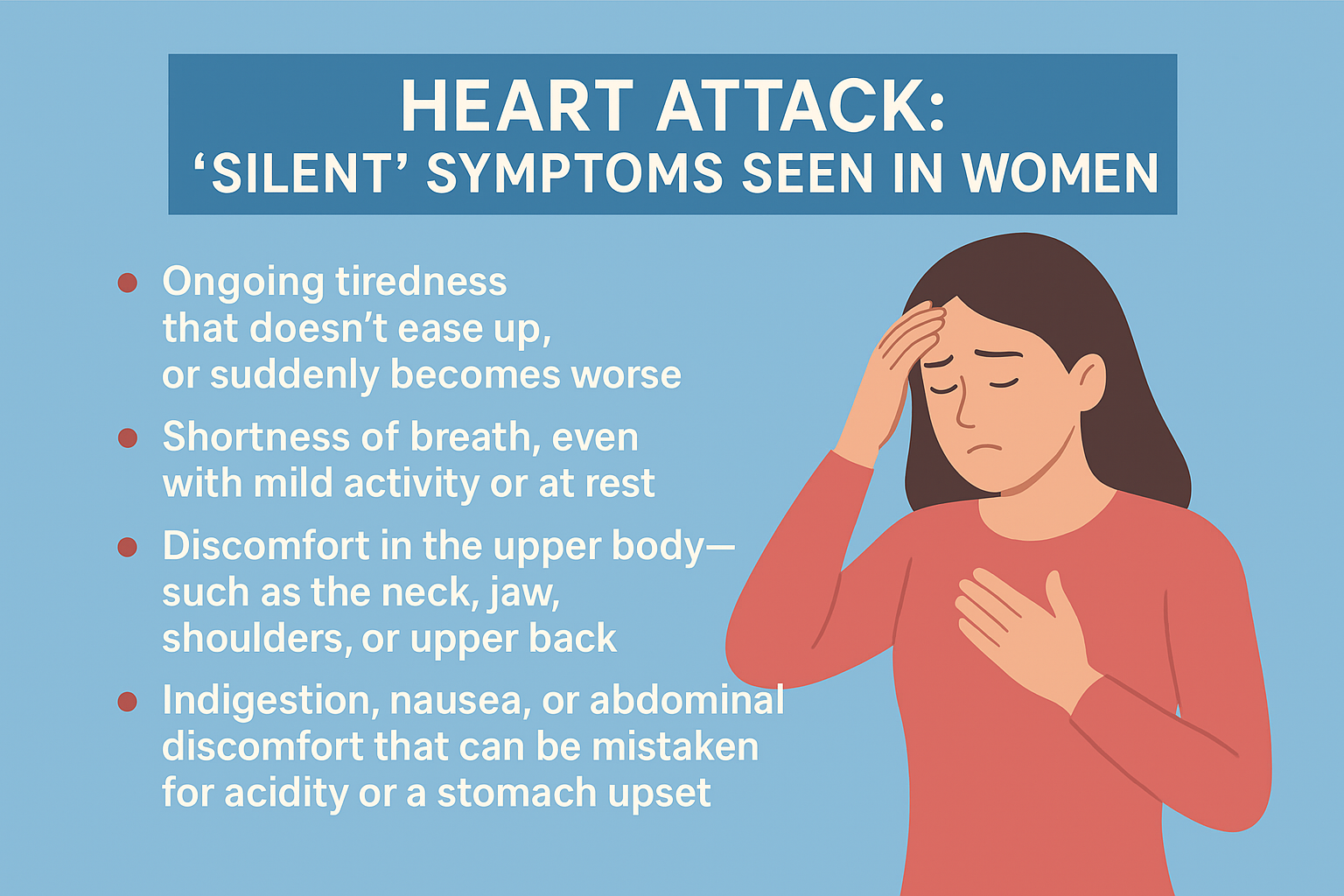
Dr Ravindranath Reddy: The warning signs of heart attacks in women can be surprisingly subtle. Most women don’t get the kind of severe chest pain we often see in movies. What they experience instead may be more subtle, such as:
- Ongoing tiredness that doesn’t ease up, or suddenly becomes worse.
- Shortness of breath, even with mild activity or at rest.
- Discomfort in the upper body—such as the neck, jaw, shoulders, or upper back.
- Indigestion, nausea, or abdominal discomfort that can be mistaken for acidity or a stomach upset.
- Lightheadedness or dizziness without obvious cause.
Because these symptoms don’t scream “heart attack,” women may dismiss them as stress, gastritis, or even aging. But if these issues appear suddenly, are severe, or feel different from a woman’s usual state of health, they should not be ignored.
How can women advocate for themselves if they suspect something is wrong, even without classic symptoms?
Dr Ravindranath Reddy: The most important step is to trust your instincts. If a woman feels that something is not right—whether it’s breathlessness, fatigue, or unusual discomfort—she should not downplay it. When seeking medical help, it helps to clearly describe what feels “different” rather than using vague words. For example, saying, “I feel breathless after walking just a few steps, which is new for me,” gives doctors a clearer picture. Women should also be firm about requesting appropriate tests like an ECG or troponin levels if there’s a suspicion of heart trouble, rather than accepting a generic explanation of stress or acidity. Mentioning a family history of heart disease, or risk factors like diabetes, high blood pressure, or smoking, is just as important. Above all, self-advocacy means asking questions without hesitation, seeking a second opinion if necessary, and making sure one’s concerns are heard and taken seriously.
What screenings or lifestyle steps can women take to reduce their risk of a silent heart attack?
Dr Ravindranath Reddy: Prevention is the strongest defense. Women should undergo regular health checks—blood pressure, blood sugar, cholesterol, and body weight monitoring—especially after the age of 35 or earlier if there’s a family history of heart disease. Tests like ECG, echocardiogram, or treadmill studies are usually suggested for women who carry a higher risk. Just as important are everyday choices—eating more fruits, vegetables, and lean proteins while cutting back on processed foods lays a strong base for heart health. Adding at least half an hour of moderate exercise on most days, keeping weight under control, avoiding tobacco, and limiting alcohol intake all support heart health. Managing stress is equally essential, as long-term stress quietly increases cardiac strain. Women after menopause should be especially cautious, since their heart risk rises considerably. Together, regular screening and healthy daily habits can go a long way in lowering the chances of a silent or late-detected heart attack.